The presence of jaundice in a child can be a
useful indicator of occult pathology. The finding of icterus should set in
motion a careful diagnostic search to elucidate the cause. The ultimate goal,
to identify precisely the cause of the clinical syndrome, may rest in some
cases with the longitudinal caregiver. In all cases, however, the emergency
physician at first visit must separate patients whose admission can be
temporized from those who require urgent intervention and/or immediate
hospitalization.
PATHOPHYSIOLOGY
Unconjugated bilirubin is largely a product of
converted heme from senescent red blood cells. Unconjugated bilirubin is
transported from extrahepatic reticuloendothelial cells to the liver, bound to
albumin. Albumin is detached as the bilirubin gains entry into the hepatocyte.
In the liver cell, bilirubin is conjugated with glucuronide by the action of
uridine diphosphate glucuronyl transferase. The soluble conjugated
diglucuronide then is secreted across the canalicular membrane into the bile.
In the intestine, as a result of the activity of bacterial flora, bilirubin is
converted to urobilinogen. A portion of urobilinogen is reabsorbed into the
portal circulation and is taken up by the liver cells, only to be reexcreted
into the bile. A small percentage of urobilinogen escapes into the systemic
circulation and is excreted in the urine. The unabsorbed urobilinogen is
excreted in the stool as fecal urobilinogen.
In hepatocellular disease, the damaged liver
may be unable to excrete the conjugated bilirubin produced in normal amounts.
Or, in the absence of hepatic damage, regurgitation into the plasma of
conjugated bilirubin may result from functional cholestasis, disruption of the
hepatic architecture, or extrahepatic biliary obstruction. In most instances of
jaundice primarily related to hepatic disease, the plasma exhibits elevated
concentrations of unconjugated and conjugated bilirubin. Overt mechanical
obstruction of bile excretion leads to raised plasma levels of conjugated
bilirubin, and only as secondary liver damage occurs do unconjugated bilirubin
levels rise.
DIFFERENTIAL DIAGNOSIS
Conjugated hyperbilirubinemia is defined by a
conjugated bilirubin level higher than 1 mg per dL if the total bilirubin is
less than 5 mg per dL or the conjugated bilirubin level represents more than
20% of the total bilirubin if the total bilirubin is higher than 5 mg per dL.
Conjugated hyperbilirubinemia, indicating cholestasis, is considered
pathological. Cholestatic jaundice may be congenital or acquired. The
differential diagnosis includes a variety of structural defects, infections,
hepatotoxins, inborn errors of metabolism, and familial syndromes (Table 41.1).
Although only a few diseases commonly cause conjugated hyperbilirubinemia
(Table 41.2), all are serious. In addition, several less common conditions are
important considerations because they are life threatening (Table 41.3).
EVALUATION AND DECISION
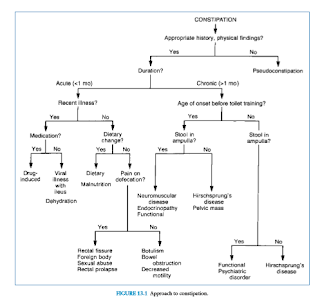
It is convenient to divide the approach to
patients with conjugated hyperbilirubinemia by age, focusing first on those
younger than 8 weeks old and then on those who are older (Fig. 41.1). A
majority of children who eventually develop lifethreatening or chronic liver
disease initially present in the first 2 months of life. Early physician
recognition may lead to successful treatment and a more favorable prognosis.
Infants Younger than 8
Weeks
In the perinatal period, infants develop
conjugated hyperbilirubinemia in response to a variety of conditions that may
not be encountered in older patients. The increased sensitivity to insult is a
result of different patterns of hepatic enzyme activity and liver immaturity
with regard to bile formation. Many systemic or hepatic insults may produce
perinatal cholestasis (Table 41.1). However, a small number of disorders
account for the overwhelming majority of perinatal cholestasis. They include
idiopathic neonatal hepatitis, biliary atresia, 1-antitrypsin deficiency, cystic
fibrosis, tyrosinemia, galactosemia, choledochal cyst, and perinatal infections.
These disorders can be separated by the tempo of the presentation and the
appearance of the infant.
The tempo of cholestasis is most abrupt with
the infections acquired in utero and during the birthing process. Infected
patients are more likely to present shortly after birth. Those who have
congenital infections will have a low birth weight. They present with
cholestatic jaundice, irritability, jitteriness, and/ or seizures. On
examination, microcephaly, hepatomegaly, splenomegaly, and petechiae may be
seen with the perinatal TORCHS complex. These include perinatal infections from
toxoplasmosis, other infections, rubella, cytomegalovirus (CMV), herpes
simplex, and syphilis. Jaundice may be one of the first signs of bacteremia
without apparent focus of infection or bacterial sepsis in the first few days of
life. Hyperbilirubinemia may occur antecedent to blood cultures becoming
positive and may precede findings of anorexia, vomiting, abdominal distension,
fever, hepatomegaly, or alterations in respiratory pattern or sensorium. The
precise mechanism of jaundice that complicates bacteremia and sepsis is not
completely understood. Jaundice may also be an early diagnostic sign of urinary
tract infection in the neonatal period. An increase in the conjugated bilirubin
fraction may be seen in patients who have afebrile, otherwise asymptomatic
urinary tract infection.
The tempo of icterus is subacute with the other
common causes of conjugated hyperbilirubinemia. The metabolic and hepatic
disorders have variable symptoms at onset. However, the manifestations are far
less acute than those seen in the infectious states. Infants with galactosemia,
tyrosinemia, and fructose intolerance may appear ill in the emergency
department due to metabolic derangement or secondary infection. However, they
have had an antecedent history of failure to thrive, developmental delay, and
inconstant jaundice. Unexplained fatality in the sibship or unexplained
pulmonary, gastrointestinal, neurologic, or psychiatric disturbance in other
family members may provoke diagnostic consideration.
The tempo of hepatic and biliary tree disorders
is chronic. Those with biliary atresia have intermittent, mild conjugated
hyperbilirubinemia during the first 6 to 8 weeks of life. They feed well and
thrive. Their stools may be intermittently pigmented early on and become
permanently without pigment only after 4 to 6 weeks. They have a benign
appearance and with the exception of jaundice and hepatomegaly seem otherwise
well. Those patients without a precise anatomic, genetic, or infectious cause
of cholestasis are considered to have idiopathic neonatal cholestasis or
neonatal hepatitis syndrome. They have onset of their jaundice from 1 to 30
days, with a mean of 7 days. Initially, their stool color is normal, but the
stools may become acholic after several weeks. The presence of acholic stools
may make it difficult to differentiate between obstructive jaundice causing
hepatocellular disease and that caused by obstruction of the biliary tree.
The priorities for the emergency physician are
to diagnose medically treatable infections, identify metabolic disorders for
which effective therapy is available, and detect extrahepatic obstructive
lesions that are amenable to surgical correction. The evaluation begins with
cultures of cerebrospinal fluid, blood, urine, and stool. Infants should also
have complete blood cell and platelet counts, coagulation studies, hepatic
enzymes (aspartate aminotransferase, alanine aminotransferase, and
gamma-glutamyl transpeptidase), ammonia, albumin, total protein, alkaline
phosphatase, electrolytes, blood urea nitrogen, creatinine, and blood sugar
tests. Urine should be obtained for urinalysis and tested for reducing
substances. A right upper quadrant ultrasound should be performed in order to
identify anatomic abnormalities such as a choledochal cyst. If cystic fibrosis
is suspected, schedule the patient for a sweat chloride iontophoresis or
testing for common genetic variants in the cystic fibrosis transmembrane
conductance regulator gene. Additional studies of blood and urine that they may
find useful include 1-antitrypsin, TORCHS and hepatitis B virus serology, serum
amino acids, thyroid function tests, red blood cell galactose 1-phosphate
uridyltransferase activity, and urine examination for cytomegalovirus.
Inpatient observation is appropriate in this
age group because the diagnosis can rarely be established in the emergency
department. Empiric therapy for sepsis or urinary infection is often warranted,
pending culture results.
Children Older than 8
Weeks
In the evaluation of conjugated
hyperbilirubinemia beyond infancy, it is necessary to know if there has been
exposure to contagion or a potential for sexual or vertical transmission of
infections such as hepatitis or human immunodeficiency virus. Other risk factors
for hepatitis (e.g., needle sticks, hemodialysis, transplant, transfusion of
blood products, or factor use) need to be evaluated. The physician should
pursue possible exposure to industrial toxins or foods previously implicated in
hepatic injury (e.g., carbon tetrachloride, yellow phosphorus, tannic acid,
alcohol, mushrooms of the Amanita species). The emergency physician must
inquire about use of acetaminophen, salicylates, nonsteroidal anti-inflammatory
drugs, iron salts, erythromycin estolate, ceftriaxone, rifampin,
nitrofurantoin, oxacillin, tetracycline, trimethoprim-sulfamethoxazole,
ketoconazole, diphenylhydantoin, isoniazid, and chlorpromazine. The presence of
prior episodes of jaundice, acholic stools, and/or abdominal pain may suggest
an underlying disorder, predisposing the patient to obstruction of the biliary
tree. Other historical points include the presence of fever, arthralgia,
arthritis, conjunctivitis, rash, pruritus, vomiting, diarrhea, weight loss, color
of the urine, abnormal bruising or spontaneous bleeding, and changes in mental
status. An examination that focuses on ongoing physical signs of liver disease
may result in greater accuracy in clinical evaluation of the older jaundiced
patient. These signs include skin changes (spider angiomata, excoriations,
palmar erythema) and peripheral edema. The abdominal examination should include
observations of the venous pattern, presence of ascites, mass, or peritoneal
irritation. There should be an estimation of liver size, contour, and
tenderness, as well as an estimate of spleen size. The clinician should exclude
cardiovascular dysfunctions such as hypoxemia, systemic venous congestion, and
low cardiac output. Observations should be made of mental status and
neuromuscular changes. Patients with cystic fibrosis, 1-antitrypsin deficiency,
Wilson’s disease, or inflammatory bowel disease tend to have symptoms that remit
and relax. However, slow progression is the rule. Patients with 1-antitrypsin
deficiency may have onset of respiratory or hepatic complaints at any age.
Similarly, infants who have failure to thrive from cystic fibrosis may develop
obstruction at any age in the extrahepatic or intrahepatic ducts and,
transiently or persistently, may exhibit jaundice. Patients with ulcerative
colitis and Crohn’s disease may become symptomatic intermittently with episodes
of cholestasis. The degree of hepatic derangement and expression of neurologic
abnormality is variable with Wilson’s disease. Before the diagnosis is entertained,
patients typically exhibit dysarthria, tremors, rigidity, or psychic
disturbances. Rarely, younger patients without prodromal events have acute
jaundice and hepatomegaly and progress to hepatic failure. Biliary calculi and
acute inflammation of the gallbladder are uncommon causes of conjugated
hyperbilirubinemia in the pediatric population. However, a subset
of patients is predisposed to these complications. Cholelithiasis may
complicate any of the hemolytic anemias, particularly in patients with sickle
hemoglobinopathies. These patients have increased incidence of both liver and
gallbladder disease. Liver or gallbladder dysfunction accounts for jaundice
when more than 10% of an elevated bilirubin in a patient with sickle cell
disease is conjugated. Cholecystitis may accompany a variety of acute focal
infections, such as pneumonia or peritonitis, and may occur in the course of
bacterial sepsis. In this event, shock and hyperpyrexia may divert the
clinician from the deranged biliary system. In less severe cases, fever,
nausea, vomiting, abdominal distension, and right upper quadrant pain are
prominent features of cholecystitis. Right upper quadrant abdominal mass, pain,
and jaundice constitute the classic triad in the diagnosis of choledochal cyst.
The clinical recognition may be delayed until there is a complication, such as
cholangitis. An acute, painful right upper quadrant mass associated with
jaundice may also occur in the course of acute hydrops of the gallbladder from
Kawasaki disease or systemic streptococcal infection. In the previously healthy
child, the most common cause of conjugated hyperbilirubinemia is acute
hepatitis . The illness may be abrupt in onset, with fever,
urticaria, and arthralgia as primary manifestations. More often, the illness is
insidious. Viral hepatitis is characterized by low-grade fever and
gastrointestinal complaints such as anorexia, malaise, nausea, vomiting, and
abdominal pain before the jaundice. Liver enlargement with hepatitis (A, B, C, and
non-A, non-B, non-C), varicella, herpesvirus, Coxsackievirus,
echovirus, Epstein-Barr virus, and adenovirus infection is inconstant. Hepatic
tenderness is a more reliable finding. Rarely, ascites can accompany hepatitis
virus infection. Splenomegaly is the rule with Epstein-Barr virus but is
unusual with the other agents. On occasion, hepatitis may be associated with a
distinctive erythematous papular eruption localized to the limbs
(Gianotti-Crosti syndrome). Toxic hepatitis, unlike viral hepatitis, does not
have a prolonged prodrome. Acute nausea, vomiting, and malaise are followed in
1 to 2 days by alterations in mental status and deterioration of liver
function. Most patients with toxic hepatitis will have an identifiable exogenous
precipitant. Children with fulminant hepatic failure typically experience
anorexia, nausea, vomiting, malaise, and fatigue—all symptoms indistinguishable
from those expected with viral hepatitis. The patient’s jaundice becomes more
profound and vomiting becomes protracted. Hyperexcitability, mania, and subtle
psychomotor abnormalities may be seen. Coagulopathy, ascites, and sudden
decrease in liver size are often the prelude to the development of frank
neuromuscular signs. The objectives of the emergency physician are to render
supportive care to those icteric patients with infectious and metabolic
derangements and to identify those cases in which jaundice is caused by
mechanical obstruction or hepatic failure. The impression based on a targeted
history, physical examination, and clinical algorithms can be bolstered with
the following laboratory examinations: complete blood cell count, platelet
count, coagulation profile, prothrombin time, total and direct bilirubin,
hepatic enzymes, alkaline phosphatase, electrolytes, blood urea nitrogen, and
creatinine. Urinalysis, culture, and toxicologic screen should be considered.
Chest and abdominal radiographs are indicated when there are pulmonary
parenchymal complaints or significant abdominal findings. Other laboratory tests
that are often available immediately and that may provide useful information in
specific circumstances are serum ammonia, albumin, total protein, lipid profile,
pH, and carbon dioxide. If available, abdominal sonography or computed
tomography may be helpful occasionally. In no circumstance will results of
several important blood and urine tests be of immediate use. Such studies,
which are appropriate, include antinuclear antibody, fetoprotein, and serum for
bile acids, ceruloplasmin, protein electrophoretic pattern, polymerase chain
reaction assays or serologic evidence of recent infection (e.g., Epstein-Barr
virus, mycoplasmal or hepatitis profiles). Urinary analysis includes assessment
of organic acids and copper. These investigations may be helpful, however, to
the longitudinal caregiver who must maintain a vigilant watch over the
jaundiced patient. Children older than 8 weeks with conjugated
hyperbilirubinemia should be admitted to the hospital at the time of their
presentation in all cases in which life-threatening conditions may exist (Table
41.3). Inpatient treatment is also suggested when intravenous fluids are
necessary to treat symptomatic hypoglycemia or electrolyte imbalance and when
operative intervention may prove necessary. Icteric patients who have been
diagnosed previously with confidence and who have exacerbation of their symptoms
may require admission to reappraise their status. The physician may also be
influenced to admit the patient when social factors or geographic barriers
inhibit consistent observations. Admission is also indicated for patients who
require further diagnostic intervention, such as hepatobiliary scintigraphy,
endoscopic retrograde cholangiopancreatography, or liver biopsy to arrive at a
definitive diagnosis.
Suggested Readings
Crain EF, Gershel JC. Urinary tract infections
in febrile infants younger than 8 weeks of age. Pediatrics 1990;86:363–367.
Emerick KM, Whitington PF. Neonatal liver
disease. Pediatr Ann 2006;35:
280–286.
Garcia FJ, Nager AL. Jaundice as an early
diagnostic sign of urinary tract infection in infancy. Pediatrics
2002;109:846–851.
Jacquemin E, Lykavieris P, Chaoui N, et al.
Transient neonatal cholestasis: origin and outcome. J Pediatr 1998;133:563–567.
Moyer V, Freese DK, Whitington PF, et al.
Guideline for the evaluation of cholestatic jaundice in infants:
recommendations of the North American Society for Pediatric Gastroenterology,
Hepatology and Nutrition. J Pediatr Gastroenterol Nutr 2004;39:115–128.
Suchy FJ. Approach to the infant with
cholestasis. In: Suchy FJ, Balistreri WF, Sokol RJ, eds. Liver disease in
children, 3rd ed. New York, NY: Cambridge University Press, 2007:187–194.